Grief House
Reflection on Six Months of Chaplaincy in a Trauma 1 Regional Hospital
I am in the last few weeks of my Clinical Pastoral Education (CPE) Unit. I am serving at Westchester Medical Center, a trauma 1 regional hospital north of Manhattan, NY. We are getting critical ill or trauma-injured patients from all over NYC, New Jersey, Hudson Valley and beyond. This is required as part of my rabbinic and cantorial education. And, I have been wanting to do this for a long time.
I had served at the hospital for most of the last few months but have not reported about it much because of confidentiality, as well as the tiring nature of the work.
Here are some vignettes from one stretch of seven days: kneeling bedside whispering Yehi Shalom Carlebach melody to a dying Jewish grandmother while her family whom she antagonized, cries; accompanying a black inmate with tons of medical risks self-advocating LOUDLY at staff (staff was patient, attentive and top of this, but things took time, busy floor); offering presence to a 95 year old man confused and scared after falling alone at home; a young alcohol addict experiencing homelessness utterly despaired, and clear-minded, with not being loved by anyone, outraged, abandoned by God; praying with a gay black man with total internal failures and a saintly heart.
This is the daily palette. It’s a thankless, unglamorous, invisible, low paid (my training is unpaid, as a volunteer) and utterly life changing work. I find it greatly fulfilling to be part of the this fractal of collective healing the individual. Hospital is a city dedicated to healing people. I have code-worded the hospital “Grief House,” makes it easier to communicate and delivers the appropriate punch.
I found the CPE modality invaluable for spiritual formation. The clinical time, curriculum, private and group supervision are like a washing machine for self-importance, ‘fixing-helping’ messianic tendencies, reliance on theology teaching-presenting, reliance on psychological modalities, reliance on stature, position or power. The training’s scope and time-investment is great. Ten hours a week of clinical practice easily translate to a lot more, with weekly reports writing, commute etc.
*
When I go to a room in the hospital, and meet someone at the edge of their physical & emotional capacity, I come with no established power, they may, can and do kick me out at any minute if I give them the wrong vibe. I have to rely on humility, presence, deep empathy and wits to establish a rapport that allows for grief and possibly spiritual yearning to be voiced. It is vastly different from the power dynamic I had as a congregational clergy, where I am the boss and people deferred to my power-position. It also puts me with people of different faiths, and no faiths, and I have to hone my ability in-the-moment to flow with them all, and still be present to grief and spiritual yearning. I must wrestle and clarify my own complex system of identities, encounter anti-semitism, micro aggressions, wrestle with forgiveness and fellowship. It is a laboratory for deep excavation, exploring my relationship with grief and pain, visibility, purpose and healing, so I can offer cleaner, more available presence, to others.
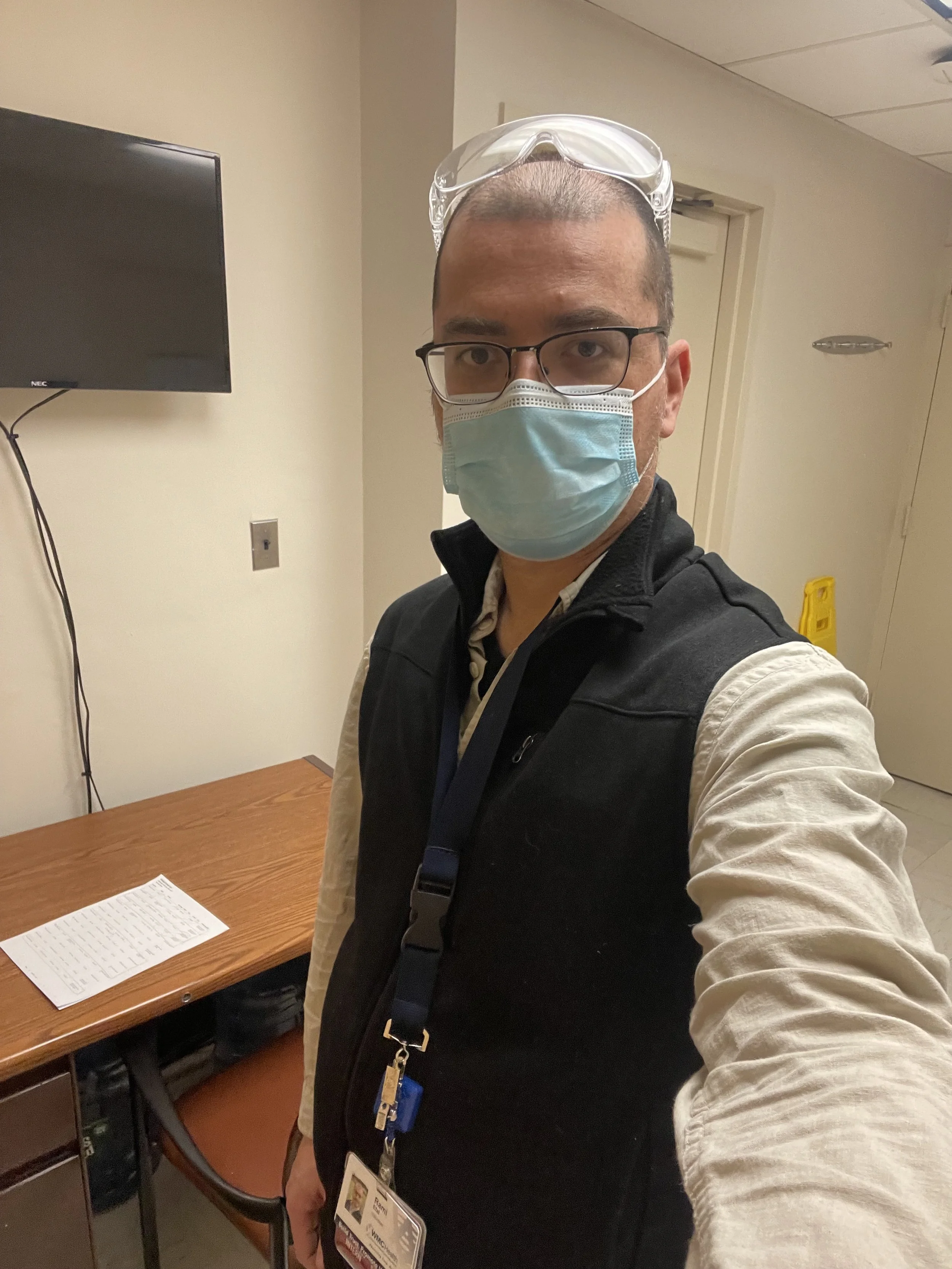
I identify as “chaplain intern,” chaplain being a christian-sourced word that lands on people in different ways depending of their own background. Wrestled with it myself for a while. (One patient’s wife whispered to me “When you become a rabbi, don’t let them call you a Chaplain!”) I wear no Jewish or Buddhist visible markers like a Jewish Kippah or a Buddhist Mala. If patients or family ask, I may share my Jewish background and Zen training. I met a Christian a patient who was abused by priests as an adolescent, and opened up only once I named my being a Jew. Others appreciate the Buddhist journey. I’ve been called chaplain, rabbi, padre, father, you name it. Sometime using a live translator through an ipad to translate, most often Spanish. I pray with all, indiscriminately. I have to move effortlessly from casual social joining to God-talk, Jesus-praying, never getting too caught up in theology, always keeping my eye on the thread of grief that is present. No one chooses to be here. Being here, everyone is losing, or missing, something.
In my visits, I noticed how often the hospital, of all places, is the only time people have to grieve over lost people or previous loss. They come here for a completely different reason, planned or by emergency, but being in a hospital with nothing to do, older or recent griefs come up to the surface. A few questions and the floodgates open.
Some patients confided that they spoke to therapists but never shared as much with them as they did with me. What is it about the chaplain? “It’s good to talk with a person of God,” one patient said. Perhaps it’s the faith, a sense of hope, Mystery? Or is that in these edge states patients are in, there is a different kind of yearning, awakening? I have a sense it has to do with silence. The silence before a question, after a question, after an answer. The permission to be. And be with grief.
To be continued - I collected many other notes I plan to share. Among the many subjects: personal supervision (private and group;) cross-cultural-religious-and-racial experience; chaplaincy-while-jewish; engaging hospital’s staff and more. I plan to explore them in further posts.
*
To close, at times I feel like a shuttle in a loom, passing through each room like hoops in a tapestry, the collective emotional fabric made by the patients, the nurses and doctors, EMT drivers & helicopter pilots landing in the helipads, and the gaggles of geese that frequent the peripheral grass patches around the Grief House.